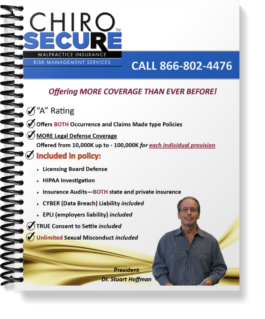
Chiropractic Malpractice Insurance that Puts You First
Your career is important to us, and that starts with protecting you when it matters most. ChiroSecure puts you and your practice first, and is dedicated to supporting you throughout your chiropractic career. Join us today to secure your chiropractic practice with comprehensive malpractice insurance coverage that is designed to fit your needs and deliver protection when you need it.
Get To Know Us
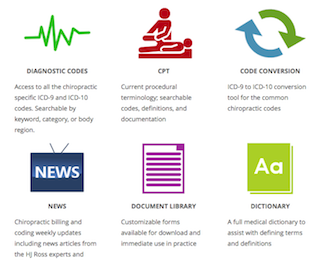
At ChiroSecure, we’re dedicated to making the hardest parts of your career as easy as possible. Don’t weigh yourself down by focusing on the negative. Work with a trusted partner that can ease the tension that comes with being a chiropractor today. Our team will provide you with the tools you need to build a successful practice, and can help you work proactively to create a safe environment where your patients can heal.